Bones muscles and joints
Published:
Scroll down for information about specific joints such as the Shoulder, Spine, Hips, Knees, Feet and Ankles.
The purpose of this section is to give explanations of why various exercises work or should work. It is based on the belief that if you know why an exercise should maintain or improve your disability or behaviour, you are more likely to do it and persist.
Exercise can prevent many age-related changes to muscles, bones and joints – and reverse these changes as well. It’s never too late to start living an active lifestyle and enjoying the benefits.
Research shows that:
- Exercise can make bones stronger and help slow the rate of bone loss.
- Older people can increase muscle mass and strength through muscle-strengthening activities.
- Balance and coordination exercises can help reduce the risk of falls.
- Physical activity in later life may delay the progression of osteoporosis as it slows down the rate at which bone mineral density is reduced.
- Whilst weight-bearing exercise, such weight training, is the best type of exercise for maintenance of bone mass in younger people, water based exercises with resistance are more suitable for elderly bones. Twisting or rotational movements, where the muscle attachments pull on the bone, are also beneficial.
- Older people who exercise in water (which is not weight bearing) may still experience increases in bone and muscle mass compared to sedentary older people.
- Stretching is another excellent way to help maintain joint flexibility.
- If you haven’t exercised for a long time, are elderly, or have a chronic disease (such as arthritis), your doctor, physiotherapist or exercise physiologist can help tailor an appropriate and safe exercise programme for you.
- If you suffer from osteoporosis, you may also be advised to take more calcium. Sometimes, medications are needed to treat osteoporosis.
The structure of joints
All exercises and swimming involve movement of joints. To see examples of such exercises in general click here. Joints are movable connections between bones. Every joint includes surfaces of the bones, a cavity and a capsule. The surfaces of the bones are covered with a layer of cartilage to stop the bones from grinding against each other. See yellow in the diagram below. The cartilage is normally thin, between 0.2 and 0.5 mm thick; but there are exceptions. For example cartilage on your kneecap could be up to 6mm thick protecting the bone beneath it. This is important where cartilage is bearing weight from above as in the spine, knees and hips. That is why we specially list exercises for the spine, knees and hips.
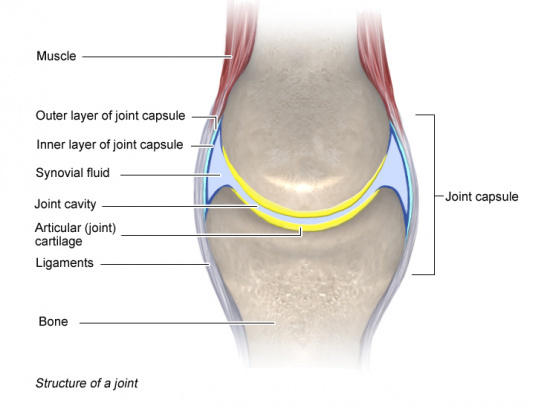
The joint capsule has an inner (dark blue line) and an outer layer (light blue line) enclosing a joint cavity that is airtight from the outside. The space it encloses is call the joint cavity or “synovial cavity”. It contains the synovial fluid. (See pale blue area.)
The inner layer contains blood vessels and nerves. The nerves relay information about pain and the position the bones are in. The outer layer of a joint capsule is made of fibrous tissue. If a joint is kept still for a long time, these fibres become shorter, particularly as you get older. As the joint capsule gets shorter it becomes less moveable and you become less mobile. That is why it is important to do gentle mobility exercises after injury, or when you have been confined to bed, or when the corona virus has left you in an armchair for a long time. Keep your joints well lubricated. If you are elderly, water in a swimming pool offers the right flexibility and resistance to maintain mobility.
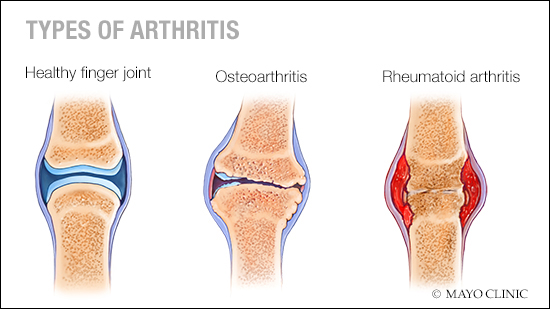
If you are elderly, you may have begun complaining of arthritis. There are two kinds. Know the difference. Osteoarthritis results from the wearing away of the cartilage protecting the ends of your bones commonly resulting from excessive weight. It is commonly associated with old age, yet in truth it usually starts in your 40s and 50s and is ignored when there is no great pain at this stage. Rheumatoid arthritis occurs when there is excessive swelling resulting from joints attacked by the person’s own immune system.
Shoulders
The shoulder is a bit complicated. There are four joints and you need to exercise all of them. To see examples click on shoulder exercises. First there is a joint between ball shape of the upper arm bone (the humerus) and the triangular shoulder blade (the scapula). It’s a ball and socket joint called the the gleno-humeral joint. So long as you keep it well lubricated with exercise, you can move your arm in a semi-sphere. In the picture, I’m trying to strengthen that joint by waving it in its full range with my hands in a child’s flippers offering some resistance.

Above the ball and socket joint is a joint between a corner of the shoulder blade (scapula) called the acromium and the collar bone (called the clavicle). This joint is called the acromio-clavicular joint.
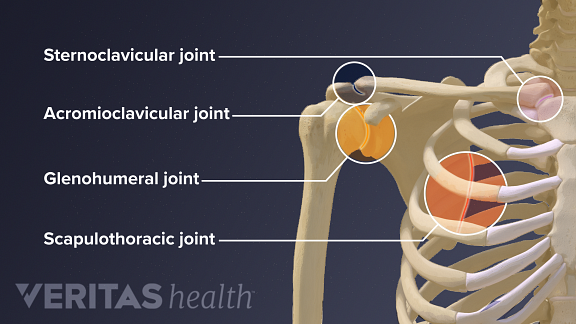
The long thin collar bone runs along the top of the shoulder and attaches in another joint at the top of the breast bone called the sternum. That attachment is another joint. You won’t be surprised that it is called the sterno-clavicular joint.
If you look at the exercises in the shoulder section, you will see they all aim to move these joints to make sure they keep working.
These bones and their joints provide a firm yet movable structure. That’s a compromise. If you think about it you will see that is necessary – secure stable structure that nonetheless allows movements of its parts. Because it’s a compromise, there is quite a lot that can go wrong in the rough and tumble of sport – fractures, tears of softer tissues, inflammation of capsules and dislocation amongst others. If you are elderly, you probably will not be attempting vigorous or violent sports now. The secret is to keep everything moving with a range of gentle exercises. Make sure you do what you can do.
Spine
To see examples of exercises for the spine click here on Spine. The spine originally evolved in fish. In fish the spine is largely horizontal in water, not weight bearing; and for propulsion it waggles its spine from head to tail a bit like a skipping rope. When the fore-runners of mammals, like cats and dogs, evolved on to dry land, they kept their spines horizontal. But when humans evolved to be vertical, our spines became weight bearing in quite a different way. The weight is bearing downwards.
The human spine is made of 33 bones called vertebrae. Those at the bottom, the lumber region, have to bear a heavier weight than those at the top. They have evolved a little bit so they are bigger and stronger. But our backbone was not originally designed to be vertical bearing these weights.
Many people have back trouble. That is partly because our spines were not designed to do the jobs we now ask them to do. They have not evolved far enough to do so. They are not sufficiently adapted to be vertical. When I was 13, my stupid PE teacher expected me to bear the weight of two other boys on my shoulders going up a ladder. There was one ginormous crack and I have had a twisted spine, a scoliosis, ever since. You may go jogging on hard tarmac roads jarring your spine every step of the way, but don’t be surprised if your knees can’t take it and your hip needs replacing when thinning bones and osteoarthritis cause trouble in old age. However I am not concerned here with treatment for all the kinds of injury.
I’m making this point: when you go swimming you are horizontal and non-weight-bearing. Your back does not bear the same stresses as in most other exercise. Swimming does not compress. It does the opposite. It stretches. Even a non-swimmer (see below) can stretch out horizontally. It is not violent. It is gentle within your ability. Furthermore, as you move your limbs in different directions using different strokes, your spine learns to adjust appropriately in different ways. The spine can meet the compromise between providing central stability and necessary adjustment.
We must now look at that stability and adjustment. In between 26 of the vertebrae is a lens shaped disk cushioning the bones from grinding against each other. The discs have a gel-filled centre and a tough fibrous outer ring that pulls the bones together against the elastic gel keeping them apart. See diagram below. When you bend your back, or tilt to one side, the gel is squashed at one side and is squeezed towards the other.
The gel-filled disk contains mostly fluid. This fluid is absorbed during the night as you lie down and is pushed out during the day as you move upright. With age, our discs increasingly lose the ability to reabsorb the fluid. They become brittle and flatter. That’s why we get shorter as we grow older. It is also why we stress the need for warm-up exercises. The discs start to dry out and no longer cushion the bones. Without the cushioning of the discs, the nerve roots or spinal cord (or both) start to get pinched or pressured. If the disks burst, the fluid may spew out touching the nerves in the spinal cord. This can be very painful and is often called ‘a slipped disc’, ‘ageing degeneration’ or ‘disc degeneration’.

Sticking out from each side of each vertebra are “spinous processes” to which ligaments and muscles are attached. See the above figure. When swimming, you stretch and bend your limbs in various directions. You breathe deeply. And there needs to be a slight adjustment between one vertebra and the next whilst holding ligaments, muscles and nerves in position. The facet joints allow vertebrae to slide relative to their neighbour. 26 small slides may mount up, but let’s face it, most humans, particularly the elderly, are not good at bending their backs and even in fish, they are not meant to bend very much. Nonetheless, the facet joints are crucial in making these slight adjustments and lying horizontal, non-weight bearing in water is the ideal way to exercise these crucial joints. The exercises for the spine are all concerned with making these adjustments regularly to keep them moving and stop arthritis cementing them rigid..
You see I want to persuade you, pool managers and other officials that, to keep mobile, elderly people need to keep all these joints in working order by regular gentle exercise. Exercising the spine is particularly important because the central nervous system affects everything else. Swimming is best because it stretches muscles all over the body when in a horizontal non-weight bearing position. However, most of the exercises we show are suitable for non-swimmers because they too need encouragement.
Hips
To see examples of hip exercises click here on Hip. In the picture below, imagine a massive weight coming down the spine because you are holding something in your arms. It reaches and is stopped by the tailbone, but then, although the weight is pressing downwards, to keep the body upright, the weight is transferred sideways on to the pelvis. If you were an architect designing this structure, you would not expect the force of gravity to go sideways like that. If God was the creator, he made a bad job of it. It relies on how well the tailbone is stuck on to the pelvis. And then the weight is transferred again sideways and downwards through the hip joint on to the leg.

Where is the greatest weakness in this structure? In spite of what I have just said, it is not in the tailbone or pelvis. They are both massive and strong. True, there may be a weakness along the joint between them. Look, the thinnest part of this structure is not the hip joint itself, but just below it at what is called the neck of femur. When your bones get weaker with age, that’s where you might get cracks or a break.
So why do your bones get weaker? Cells throughout the body are decaying and replacing themselves all the time throughout life. The problem with bones is that the replacement is not as much, or quite the same, as the wastage. There are three kinds of bone cell. Their names all begin with ‘osteo’ meaning bone. Osteocytes form compact mature bone consisting of osteons. Osteons are concentric layers of bone called lamellae, which surround long hollow passageways, the Haversian canals. Osteoblasts are bone forming cells; and osteoclasts break down and reabsorb material for wastage leaving spaces amongst what was compact bone. If replacement material coming along your blood vessels is deposited at the first spaces it finds, the centre of bones won’t be resupplied. It is the outer bone that will be re-supplied first. The centre will no longer be compact. It will be spongy and weak (also called ‘cancellous’ or ‘trabecular’ bone). Excessive spongy bone amounts to osteoporosis.

The hip joint itself is a large ball and socket joint. As you age, the joint movement becomes stiffer and less flexible because the amount of lubricating fluid inside on the ball decreases and the cartilage becomes thinner. Ligaments also tend to shorten and lose some flexibility, making joints feel stiff.
Many of these age-related changes to joints are caused by lack of exercise. Movement of the joint, and the associated ‘vibration’ of movement, helps keep the fluid moving. It is thought that exercise stimulates osteoblasts to replace bone material and reduce osteoporosis. Being inactive causes the cartilage to shrink, stiffen and reduce mobility.
Osteoarthritis of the hip and elsewhere is a common condition worldwide. It is an increasing risk in old age. It’s as if osteoblasts are dumped in the wrong place. Exercising to push away the misplaced deposits is often the only way to maintain a functioning joint. In the hip this can be particularly painful, but it is much less painful when the hip is suspended in water because then it is non-weight bearing.
There is some evidence of an inherited disposition for arthritis. Why is osteoarthritis a bigger problem for postmenopausal women than men? Women are built differently than men. The average woman’s hips are wider than her knees, as opposed to men. Also, the typical woman’s knee joints are not aligned as straight as men’s. So now we had better consider your knees.
Knees
To see exercises for the knee, click here on Knee. The knee joint is a hinge joint between the thigh bone (the femur) and the lower leg bone (the tibia), which mainly permits flexion (bending) and extension (stretching and straightening) of the leg. There can be a small amount of rotation when the leg is bent. This joint is also weight bearing on land, but this is markedly reduced when floating in the water.
The third bone is the kneecap (the patella). The patella is both formed and lies inside the quadriceps femoris tendon. In that position it provides a fulcrum to increase power of the knee extensor and also serves as a stabilising structure that reduces frictional forces applied to the femur.
The diagram below labels a number of bursae. What is is a bursa? Tendons, ligaments, muscles, and skin must glide between bones and soft tissue during joint movement. Bursae are slippery sacs of fluid that facilitate this gliding motion by providing a thin cushion and reducing friction between the surfaces.

If bursae around the knee are irritated they can become inflamed and painful and may be best treated by rest rather than exercise. The inflammation all too often results from patients being overweight. Knee replacement surgery has become very successful in reducing pain and increasing the range of movement.
Feet and Ankles
The exercises we illustrate are to maintain your mobility. To see examples click here on Feet. In particular we aim to maintain the range of ankle movements to prevent arthritis. So they are preventative, not necessarily therapeutic, but they can be. Though there is some movement from side to side, the ankle joint is a hinge joint between the tibia and fibula of the leg and the talus below. In the diagram it is called “mortise joint”.
Your feet are made for walking—and running, jumping, balancing, climbing, and more. So it’s no wonder that the human foot is complex. In the feet and ankles there are 28 bones and 33 joints all held in place by soft tissues such as more than a hundred ligaments, tendons and muscles and served by nerves and blood vessels. You demand a lot from them. They have to bear the weight of your body often for long periods every day. So it’s not surprising if you get swellings like sprains and strains from time to time.
If so rest rather than exercise. Take an anti-inflammatory like ibruprofen, elevate your foot and wrap ice in a thin towel round it. If you need to walk, firmly wrap a bandage to give support. If pain lasts more than a few days, get professional help from a physiotherapist, podiatrist or orthotist.

All of these structures work together like fine-tuned machinery to carry out two important functions: weight-bearing and propulsion. These functions require a high degree of stability. In addition, the foot must be flexible so that it can adapt to uneven surfaces. That is one reason each foot has so many bones and joints.
Let’s have a brief overview of the structures of the foot and how they work together, plus a look at some common pediatric problems that sometimes result from normal wear and tear, overuse, or injury to the foot.
The foot can be divided into three sections: the forefoot, midfoot and hindfoot. There are bones, joints, muscles, tendons, and ligaments in each section.
Bones. The forefoot is the very front part of the foot, including the toes, or phalanges. There are 14 toe bones (two per big toe and three per each of the other four), plus five metatarsals.
The first metatarsal bone is the shortest and thickest and plays an important role during forward movement. It also provides attachment to several tendons. The second, third, and fourth metatarsal bones are the most stable of the metatarsals. They are well protected and have only minor tendon attachments.
In addition to the phalanges and metatarsals, the forefoot contains two small, oval-shaped sesamoid bones just beneath the head of the first metatarsal, on the underside, or “plantar surface”, of the foot. This is also held in place by tendons and ligaments.
The forefoot meets the midfoot at the five joints with five irregularly shaped bones called the tarsals. The clinical names for these bones are the navicular, cuboid, and medial, intermediate, and lateral cuneiforms. Together they form the arch of the foot. The arch of the foot plays a key role in weight-bearing and stability.
There are only two large bones in the hindfoot section of the foot: the talus and the calcaneus. The largest of these, the calcaneus, forms the heel of the foot. You know where the heel is, but it is hidden in the diagram because, from that viewpoint, the talus rests on top of it and forms the pivoting joint of the ankle.
Joints. Turning now from the bones to the joints, a joint is formed at the junction between two or more bones. If you look at the diagram, each big toe has two joints. They have long names using the names of the bones they join, the metatarsophalangeal joint and the interphalangeal joint. The other four toes on each foot have three joints each: the metatarsophalangeal joint at the base of the toe, the proximal interphalangeal joint in the middle of the toe, and the distal phalangeal joint—the joint closest to the tip of the toe.
The muscles that control the movements of the foot originate in the lower leg and are attached the bones in the foot with tendons. These are the main muscles that facilitate movement in the foot. This is what they do.
- Tibialis posterior (supports the foot’s arch)
- Tibialis anterior (allows the foot to move upward)
- Peroneus longus and brevis (controls movement on the outside of the ankle)
- Extensors (raise the toes to make possible to take a step)
- Flexors (stabilize the toes and curl them under)
Tendons and ligaments. The best known tendon of the foot is the Achilles tendon, which runs from the calf muscle to the heel. It is the strongest and largest tendinous structure in the body. 2 The Achilles tendon makes it possible to run, jump, climb stairs, and stand on your toes.
Other important tendons in the foot include the tibialis posterior (posterior tibial tendon), which attaches the calf muscle to the bones on the inside of the foot and supports the arch of the foot, and the tibialis anterior (anterior tibial tendon), which runs from the outer tibia to the first metatarsal and surfaces of the median cuneiform tarsal, which allows for dorsiflexion—bringing the toes toward the shin.
These are the primary ligaments of the foot:
- Plantar fascia—The longest ligament of the foot, the plantar fascia runs along the sole of the foot from the heel to the toes to form the arch of the foot, provide strength for walking and assisting with balance.
- Plantar calcaneonavicular ligament—This is a ligament of the sole of the foot that connects the calcaneus and navicular and supports the head of the talus.
- Calcaneocuboid ligament—This is the ligament that connects the calcaneus and the tarsal bones and helps the plantar fascia support the arch of the foot.
Common problems Given how many moving parts there are in the human foot and how many thousands of miles this amazing body part logs in a lifetime it’s not surprising that structures within it can be subject to injury or overuse.
Like any body part that’s made up of bone, muscle, and connective tissue, the feet are subject to certain conditions that can affect any other extremity, limb, or the spine, including:
- Sprains, strains, and pulls affecting muscles or ligaments
- Tendinitis (when a tendon becomes overstretched or torn)
- Bone fractures and breaks
- Osteoarthritis (which is particularly common in feet, especially in the joints that connect the toes to the midfoot)
- Rheumatoid arthritis
Feet can also be affected by medical conditions that aren’t specific to them, such as diabetes, gout (in which crystals of uric acid form in a joint), infections (such as athlete’s foot and fungal infection under the toes).
There are problem unique to the foot itself. As the largest bone in the foot, the heel (calcaneus) is especially prone to injury caused by faulty biomechanics. That is walking in unsuitable ways. A common example is bony growths on the underside of the calcaneus, called heel spurs. They can cause severe pain when standing or walking. Plantar fasciitis results from microtears in the thick fibrous tissue on the underside of the foot, extending from the heel to the ball, caused by overstretching. Symptoms include pain in the heel and arch that’s often worse in the mornings. P
Bunions form when the bones in the foot become misaligned, often due to pressure caused by wearing shoes that don’t fit well or that squeeze the toes tightly together over a long period of time. The big toe can angle so far inward that it actually crosses under or over the adjacent second toe, causing a secondary misalignment called a hammertoe usually, a painful callous forms on top of the second toe.
Fallen arches or flat feet, this is a deformity in which the arc of the underside of the foot straightens out, often so completely that the entire sole of the foot comes in contact with the floor. The result can be pain in the midfoot area, swelling of the ankle and arch of the foot, and even hip, knee, or lower back pain. Fallen arches can be congenital (meaning a person is born with the condition), but more often develops as a result of age or injury. Between 20% and 30% of people have some degree of flat-footedness.
Metatarsalgia is the name for pain under the ball of the foot often caused by increased pressure on this area because of certain types of shoes, arthritis, nerve compression, fractures or tears in ligaments. Morton’s neuroma is a problem iwhere compression on a nerve in the ball of the foot causes burning, tingling, and pain near the third and fourth toes. High heels are often the culprit..
Diagnosis In order to diagnose common problems related to the anatomical structures in the foot, a doctor—usually an orthopedic specialist—will examine the outside of the foot to look for symptoms such as swelling in specific areas and deformities in the shape of the foot and other external signs.
However, for a specific diagnosis, it usually is necessary to take a look inside of the foot using some sort of imaging test. A standard X-Ray can confirm a bone fracture or arthritis damage. If more detail is needed, magnetic Resonance Imaging (MRI) technique which uses a powerful magnet and a computer. Or a computed tomography (CT) scan can construct images by combining multiple X-rays.
WEFTE is particularly concerned with maintaining mobility amongst the elderly. Avoiding problems in the feet and ankles is important to maintain mobility. Without mobility you are likely to lose your independence. Exercises in water do not necessarily cure those problems, but they make the feet more malleable. If problems persist, get professional help.